The Present and Future of ACL Rehabilitation: Force Plate Testing in Outpatient Clinics
- Carlos Jimenez
- Dec 29, 2024
- 4 min read
The landscape of rehabilitation after Anterior Cruciate Ligament Reconstruction (ACLR) is evolving, and vertical jump testing using force plates is at the forefront of this change. As highlighted in a recent systematic review and meta-analysis, force plate analysis offers precise insights into post-ACLR deficits that conventional tools often overlook. While this technology has been primarily used in elite sports settings, it’s only a matter of time before force plates become essential and accessible in outpatient clinics. Link to Lower limb assessment
Persistent Deficits Post-ACLR: What the Research Tells Us
The systematic review evaluated 42 studies encompassing over 2,300 participants and revealed significant, persistent impairments in lower-limb performance even after rehabilitation. Key findings include:
1. Bilateral Deficits:
• Peak Forces: Reconstructed limbs displayed significantly lower peak eccentric, concentric, and landing forces compared to the uninjured contralateral limbs during bilateral countermovement jumps (CMJs).
• Impulse Measures: Both eccentric and concentric impulses (force applied over time) were reduced in reconstructed limbs, with standardized mean differences (SMDs) ranging from -0.56 to -0.80. These metrics reflect impaired ability to generate and absorb force efficiently.
2. Unilateral Weakness:
• Reconstructed limbs demonstrated lower jump heights and reactive strength indices (RSI) during unilateral CMJs and drop vertical jumps (DVJs) compared to uninjured limbs and healthy controls.
• Reconstructed limbs had significantly longer contact times, suggesting slower and less efficient movement strategies.
3. Chronic Asymmetries:
• Even during bilateral tasks, offloading strategies were evident, with reconstructed limbs contributing less to the takeoff and landing phases.
• These asymmetries may increase the risk of re-injury, particularly to the contralateral limb, as reconstructed individuals often rely more heavily on the uninjured side.
4. Slow Recovery Over Time:
• Jump height and RSI showed gradual improvement over time post-surgery but often failed to fully normalize, especially when compared to healthy controls.
• Metrics like concentric impulse, a critical determinant of jump height, revealed persistent asymmetries long after the expected recovery period.
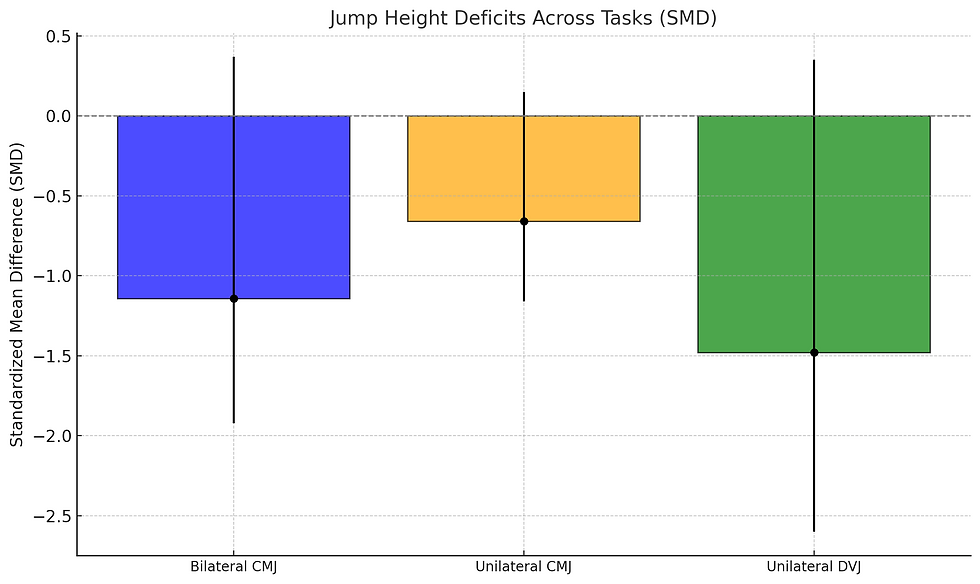
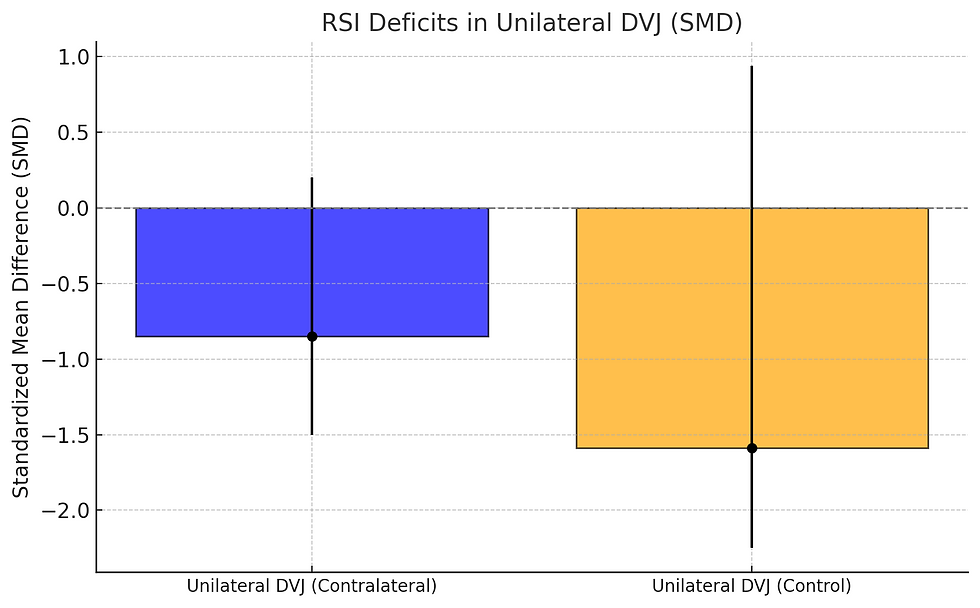
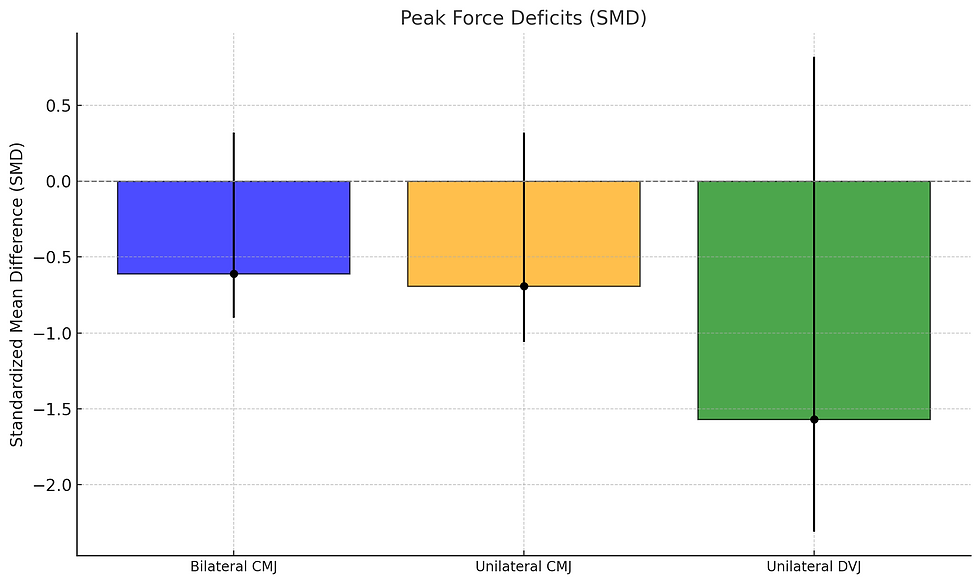
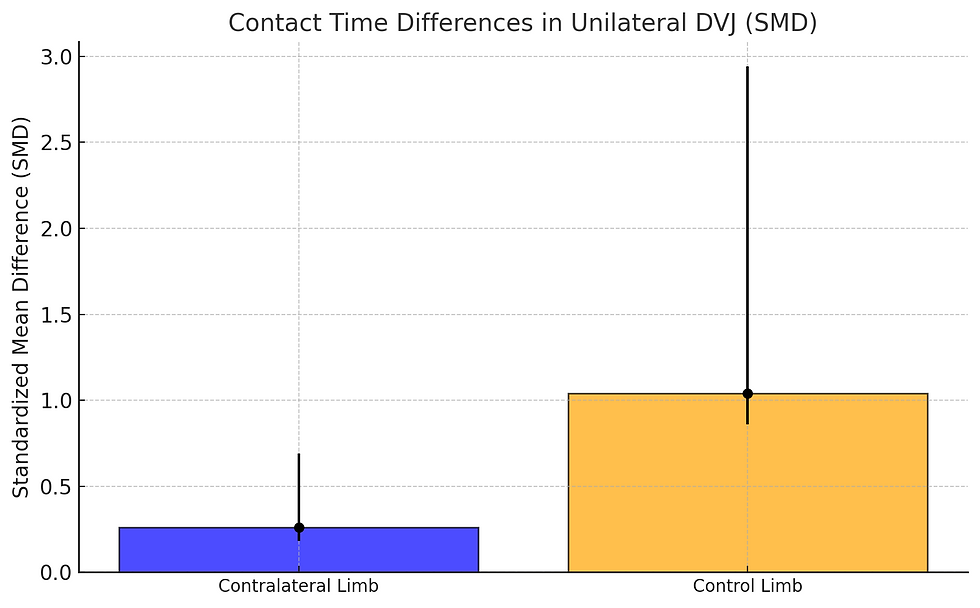
Visualizing the Evidence: Key Deficits in Vertical Jump Performance Post-ACLR
To better understand the impact of ACL reconstruction on lower-limb performance, the following graphs highlight the significant deficits observed in jump height, reactive strength index (RSI), peak forces, and contact times. These visualizations provide a clear depiction of the challenges faced during rehabilitation and the potential role of force plate testing in addressing these issues.
1. Jump Height Deficits Across Tasks:
• Highlights significant reductions in jump height across bilateral CMJ, unilateral CMJ, and unilateral DVJ, with the greatest deficit in unilateral DVJ.
2. Reactive Strength Index (RSI) Deficits in Unilateral DVJ:
• Shows reduced RSI values for reconstructed limbs compared to both contralateral and control limbs, emphasizing the efficiency deficit in the stretch-shortening cycle.
3. Peak Force Deficits:
• Demonstrates lower peak eccentric and concentric forces during various jumping tasks for reconstructed limbs.
4. Contact Time Differences in Unilateral DVJ:
• Reconstructed limbs exhibit longer contact times, indicating slower movement strategies compared to contralateral and control limbs.
Why Force Plate Testing Matters
Force plate analysis provides clinicians with quantitative data that are difficult to capture through traditional return-to-play tests, such as hop distance or subjective evaluations. For example:
• Ground Reaction Forces (GRF): Detailed insights into eccentric and concentric force production during jumping and landing tasks.
• Impulse Metrics: These measures highlight deficits in force generation and absorption, critical for explosive movements in sports.
• Reactive Strength Index (RSI): A valuable marker of stretch-shortening cycle efficiency, correlating strongly with athletic performance in sprinting and cutting maneuvers.
By identifying these deficits, clinicians can design more targeted interventions to restore symmetry, strength, and neuromuscular control, ultimately reducing the risk of re-injury.
The Path to Accessibility in Outpatient Clinics
Historically, force plate testing was reserved for elite sports facilities due to cost and complexity. However, technological advancements are rapidly changing this landscape:
• Portability: Compact and user-friendly force plates are now available, making them practical for outpatient settings.
• Affordability: Lower-cost options are emerging, enabling clinics to invest in this game-changing technology without prohibitive expenses.
• Patient Engagement: Objective, visual data from force plates enhance patient understanding and motivation, fostering adherence to rehabilitation protocols.
A Game-Changer for Outpatient Care
Incorporating force plates into outpatient clinics is no longer a luxury—it’s becoming a necessity. With their ability to quantify deficits that persist long after conventional rehabilitation ends, force plates can revolutionize post-ACLR care. Outpatient clinics that adopt this technology will be at the cutting edge of sports medicine, offering enhanced precision in assessment, improved patient outcomes, and better return-to-play decisions.
Reference:
Dutaillis, B., Diamond, L. E., Lazarczuk, S. L., Timmins, R. G., & Bourne, M. N. (2024). Vertical jump testing after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Medicine & Science in Sports & Exercise, 56(2), 181–192. https://doi.org/10.1249/MSS.0000000000003298
Comments